16 year-old Swara Kulkarni was the runner-up for the Harbinger Prize in Science
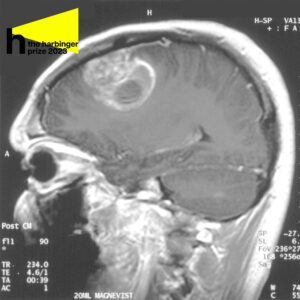
Sagittal MRI with contrast of a glioblastoma in a 15-year-old boy
October 27, 2023
Glioblastoma. What’s being done about the cancer with over a 90% mortality rate?
The word ‘glioblastoma’ is seldom one that rings a bell. It describes a type of cancer which ravages the brain, causing cell death. The worst part; there’s only been a 6.9% five-year survival rate.
Let’s break it down. Glioblastoma originates from astrocytes and oligodendrocytes, supporting glial cells within the brain. Mutations in the genome cause these cells to turn harmful.
Although the exact event that sparks the beginning of these tumors is unknown, scientists believe that as more mutations occur, the malignant tissue starts invading the healthy tissue. This marks the beginning of the tumor progression.
Glioblastoma is notorious because of its thin branches that spread through the healthy brain tissue and makes the tumor extremely difficult to remove – a part of the tumor visible to the naked eye is only a small fraction of the entire glioblastoma. What grows underneath the healthy tissue is often the most malignant and unpredictable, because neural pathways aid the tumor in spreading to opposite sides of the brain.
While removing a tumor, surgeons often cut out healthy tissue surrounding it (called the margin) to be sure they eliminate as many damaging cells as possible. Glioblastoma often originates in the frontal and temporal lobes of the brain, critical for processing memory, emotions, auditory information, as well as sensory input. Neurosurgeons have to navigate meticulously to limit the damage to the brain.
Surgery, however, is just one way to treat glioblastoma – radiation and precision medicine both have noted successes, and researchers are working on several other ways to target the cancer.
Radiation works when the cancerous cells are actively growing and dividing, killing them during that process. However, stem cells of tumors are not growing, which does not render them susceptible to chemotherapy or radiation.
Some scientists expressed concerns that radiation is ineffective, as it may facilitate the return of tumors.
Sandeep Burma, radiation biologist at the University of Texas Health Science Center warned that as radiation treatment increases, senescence occurs, because brain cells are aging prematurely, thus causing cancer to grow more aggressively.
“The recurrent tumor could be, perhaps, even more resistant to the second line of therapy,” Burma said in an interview with 16 News Now.
Precision medicine is another way to treat glioblastoma. Selinexor – a drug used to shrink the size of a brain tumor by about a third – has shown promising results in clinical trials.
Selinexor inhibits exportin-1, a protein exporter that stretches from the nucleus to the cytoplasm, which is often overexpressed in cancers, including glioblastoma. Effectively, selinexor suppresses tumor proteins in the nucleus before they can spread.
However, the drug needs further trials – for now, it is approved by the U.S. Food and Drug Administration (FDA) only to treat refractory multiple myeloma and relapsed/refractory diffuse large B-cell lymphoma.
Professors Raman Bahal of the UConn School of Pharmacy and Mark Saltzman of Yale seek another cure by taking bioadhesive nanoparticles and attaching them to the site of the tumor.
Learn more:
The particles slowly release synthesized peptide nucleic acids which target overexpressed micro RNAs known as ‘oncomiRs’. When the nanoparticles attach, they stun tumor progression.
Saltzman and Bahal’s cure sets them apart because it targets two oncomiRs, speeding up the death of malignant cells. This new technology would be inserted through surgery and supported with radiation which increases the sensitisation of the cells to therapeutic techniques.
The Tumor Treating Fields (TTF) technology has made breakthroughs regarding the progression of glioblastoma.
Electrical signals are transmitted from the scalp and interfere with the ability of cancerous cells to divide. When a cancer cell is ready to multiply, the chain of proteins that are pulled apart is disrupted. Over time, these cells self-destruct, which causes the tumor to shrink in size.
The transducers are attached to wires connected to the patient’s head with bandages. Notably, the device allows people to live normally while receiving treatment.
All these treatment options combined are responsible for only 10% survival rate over the past five years. It is clear how much research is needed – and the big question is how to reach the root of the problem and prevent glioblastoma from taking hold in the first place.
With 12,000 people being diagnosed with glioblastoma every year, this is truly a cause worth fighting for.